What is it?
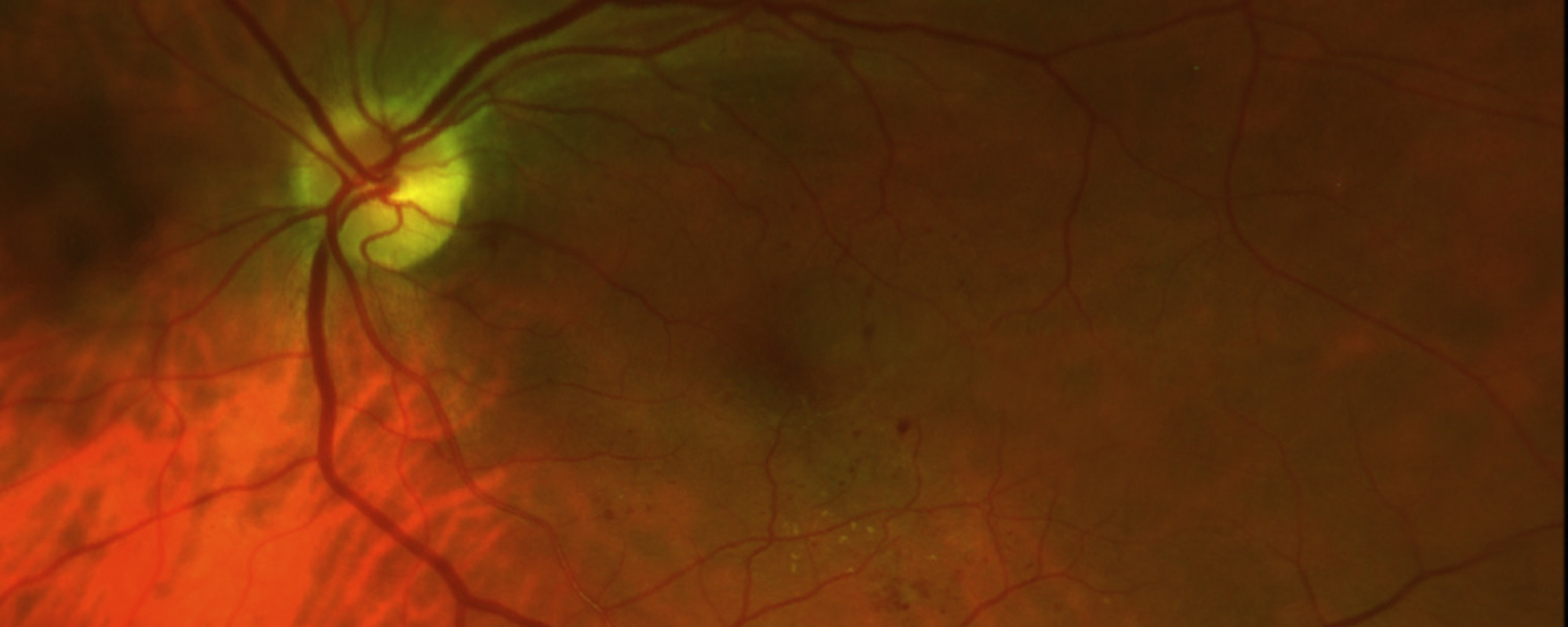
A Retinal Detachment is a disease of the retina, the structure of the eye that detects light. They often occur in nearsighted patients but may occur in anyone. It is caused by the vitreous (the clear jelly in the middle of the eye) tugging on the retina to create a retinal hole or tear. Fluid then dissects underneath the retina, separating it from the back of the eye. Macula-on detachments are emergencies where the center of your vision has not been effected yet. Macula-off detachments are detachments that already have dissected under the center part of your vision.
How do I fix it?
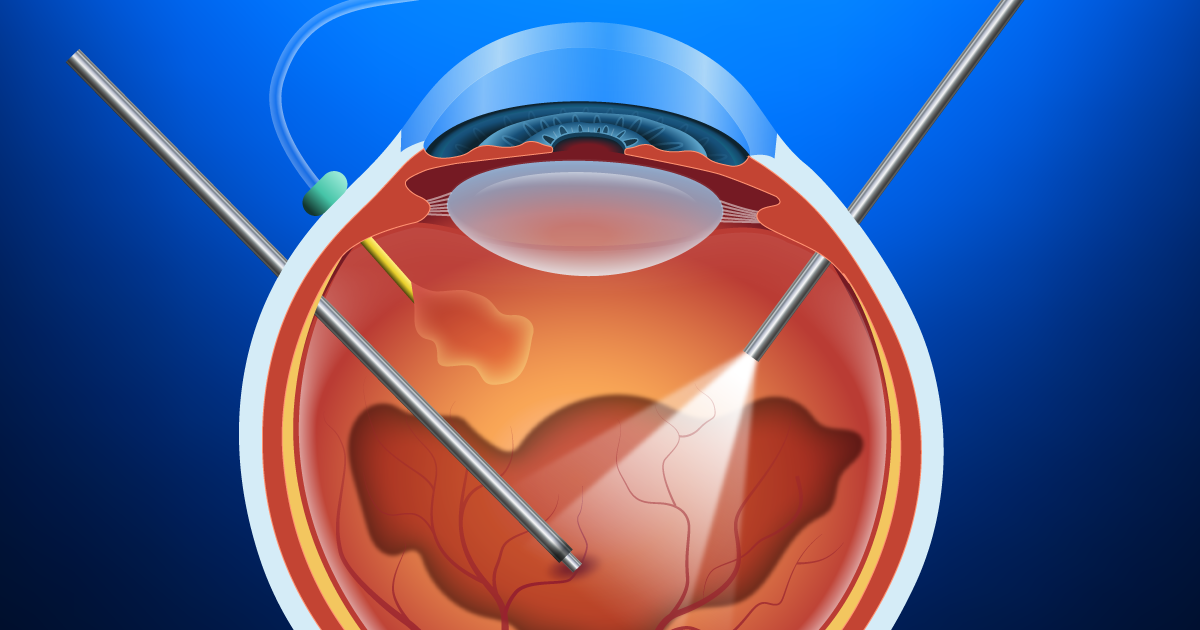
Option 1 – Vitrectomy Surgery
First, your retina surgeon carefully removes the vitreous jelly from the eye, replacing it with saline fluid. Then, your surgeon removes the fluid from underneath the retina which allows it to sit back again on the back of the eye. The surgeon will then fill the eye with air or a gas bubble to act as a “eye cast”, to allow the retina to heal properly after the surgery. The surgeon then lasers or applies a freezing treatment to “spot weld” the area of the retinal break. Often, your surgeon will place a scleral buckle around the eye to squeeze the eye slightly in the middle to reduce tension on the retina. Rarely, your surgeon may use a semi- permanent eye cast such as silicone oil. The surgery usually takes about 2-3 hours to complete.
After the surgery, your surgeon may ask that you position your head to help your retina heal properly.
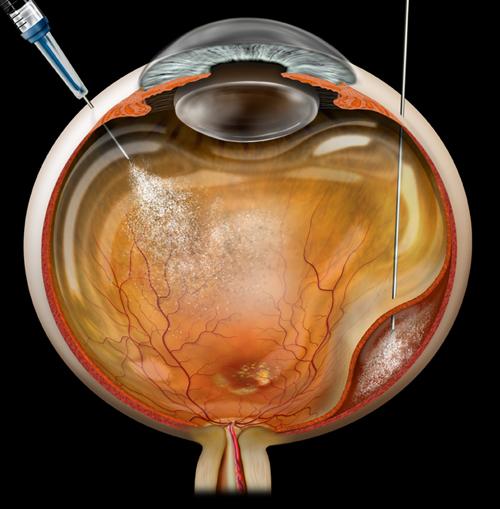
Option 2 – Pneumatic Retinopexy
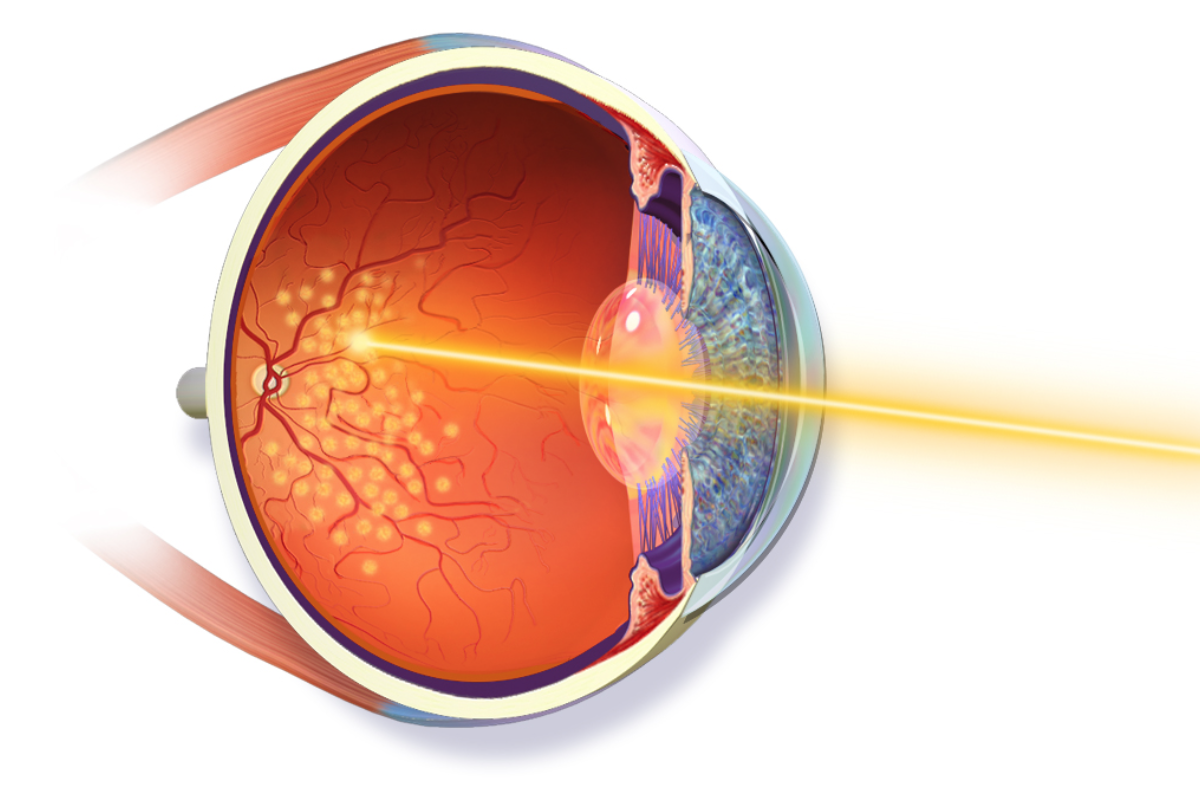
Your retina surgeon may choose to perform a pneumatic retinopexy. In some patients, injecting a long acting gas (perfluoropropane) into the eye helps the retina absorb the fluid underneath it. This procedure can be done in the office.
Next, once the retina is flat against the back of the eye, your surgeon performs a cryopexy (freezing treatment), or a laser to spot weld the retina, and prevent further detachments. This procedure is usually 80% successful, but avoids cutting surgery.
What can I expect afterwards?
The gas bubble will make your vision extremely blurry until your eye absorbs the gas. This may take from 2-4 weeks for sulfur hexaflouride gas, or 4-6 weeks for perfluoropropane gas. Silicone oil will remain in the eye, until it can be surgically removed, usually in 3 months.
Also, your eye may be red, swollen, and irritated from the surgery. This is all normal, and may blur the vision as well.
There are no guarantees that your vision will improve. However, in several studies, most patients who had retinal reattachment surgery for macula- on detachments improved considerably. Even those patients with macula-off detachments operated on within 2 weeks will on average improve to 20/50.
What drops will I take after the surgery?
Ofloxacin – four times a day for the first week after surgery
Prednisolone- four times a day for two weeks, then three times a day for a week, then two times a day for a week, then one time a day for a week.
What are the risks of the surgery?
Most of our patients who have not had cataract surgery will likely develop cataracts within a year of the surgery. This is a common finding after vitrectomy surgery and is to be expected in most patients.
Infection may also occur, but it is extraordinarily rare. Pain is very common, but is often controlled with pain medications given after the surgery. There will be no pain during the surgery since you will be given an anesthetic injection around the eye and may even be asleep or in a twilight state for the surgery. Increases in eye pressure may also occur, but is usually easily controlled with eye drops.
When do I come back for followup?
Our usual followup plan includes visits at one day, one week and one month after the surgery. We usually suggest waiting at least 3 months before getting new glasses. If you have not had cataract surgery, then we will likely suggest cataract surgery from 3 months to a year after the surgery, if needed.